Ceramic bone injection enhances treatment of osteoporosis fractures
A ceramic bone-substitute injection holds promise to treat osteoporosis patients with fractures, report scientists at Lund University, Sweden.
Instead of only conventional surgery with screws and metal plates, hydroxyapatite (HA) – a natural component in bone tissue – would be injected around the orthopaedic implant.
Associate Professor Deepak Raina, who led the study, claims the material solidifies within minutes and immediately improves bone anchorage strength.
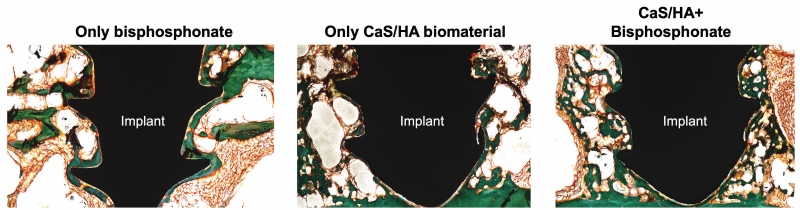
In a second step, the patient is then injected with bisphosphonate, which reaches the bone mineral via the bloodstream and reportedly binds and activates new bone formation around the implant.
This is said to be the first time that these treatments have been used together rather than in isolation.
'If you have reduced bone quality, due to osteoporosis, you have not only an increased risk of fracture but also an increased risk of implant failure, if the fracture needs an operation. Screws may become loose or cut through the weakened bone tissue,' says Magnus Tägil, Professor of Orthopaedics at Lund University and Consultant at Skåne University Hospital.
Raina adds, 'Hydroxyapatite or tricalcium phosphate, both of which are clinically used calcium phosphate materials, first provide biomechanical advantages by increasing the anchorage of the fracture fixation screw to poor quality osteoporotic bone.
'Secondly, they act as a recruiting moiety for systemically administered bisphosphonates. When the systemically administered bisphosphonate seeks and binds to the synthetic HA, the HA particles are biologically activated and transform into living bone.'
This study reportedly shows an injectable calcium phosphate ceramic can consistently and safely be applied at the interface between a hip screw and osteoporotic bone during surgery.
Results suggest that the immediate anchorage of the screw-bone interface increases by up to 400% using the biomaterial when compared to no augmentation.
To achieve an 'optimal immediate mechanical anchorage and an appropriate bone regeneration response', the surgical method for applying the ceramic material and the timing of administering the bisphosphonate were optimised and are covered by pending patents. Moroxite F, Sweden, is the industrial partner.
This method also has wider benefits. Raina says, 'Osteoporotic hip fracture patients have a 3-7% risk of reoperation, with 20-40% mortality within the first year after the fracture and significantly higher in case of a reoperation. Moreover, the quality of life is significantly reduced and the patients do not return to the same level of activity as prior to the fracture.
'It is envisaged that, with the proposed treatment, a 50% risk reduction in the reoperation rates would be beneficial from both health economics and patient perspective.
'A larger efficacy fracture study on osteoporotic patients will be necessary to prove the reduced risk of reoperations.'
They are also working on a small-scale feasibility study for vertebral compression fracture patients.
Raina notes, 'The demographic changes and the ‘age-quake’ are going to be overwhelming for the healthcare system and one potential way to tackle the challenge is to have top-notch surgical techniques and drug treatment available to minimise societal costs and human suffering.'







