3D-printed biomesh inhibits inflammation post hernia repairs
A 3D-printed biomesh made with a phosphate crosslinked polyvinly alcohol (X-PVA) could be the answer to preventing complications following hernia repairs.
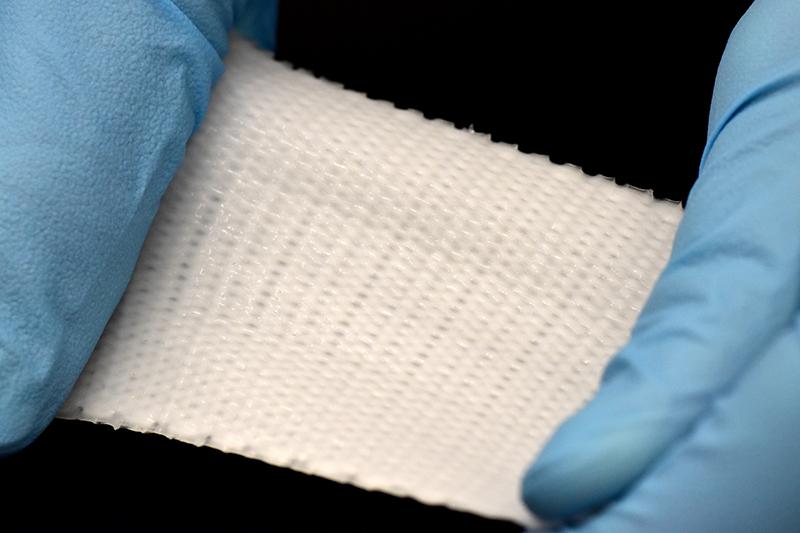
The non-absorbable mesh can be surgically implanted and sutured to repair soft tissue defects and injuries.
In a study from the Baylor College of Medicine, USA, researchers have found that the biomesh is pliable yet mechanically robust and acts as an inflammation trap by capturing pro-inflammatory cytokines. It can also modulate inflammation and minimise visceral adhesion formations.
‘We designed the biomesh to yield an elastic modulus that closely matches with that of the abdominal muscles where it will be implanted during the hernia repair,’ says Dr Crystal Shin, Assistant Professor of Surgery at Baylor. ‘Matching elastic modulus improves its compliance. The biomesh can provide adequate mechanical strength and withstand abdominal pressure.’
Shin notes that the approach to developing the biomesh is quite different to currently available surgical meshes. ‘For example, PROLENE, a commonly used prosthetic mesh is made with polypropylene. This mesh when implanted can induce foreign body reaction and inflammation, which can lead to adverse complications such as visceral adhesion, hardening and shrinking of the mesh over time, often requiring additional surgical interventions.’
She explains that chemical modification of the new biomesh gives a negative surface charge. This inherent property means it can ‘capture’ excess pro-inflammatory cytokines that are positively charged. This inflammation-modulation reduces visceral adhesions, improving recovery.
‘We used a crosslinker, sodium trimetaphosphate (STMP) to improve the stability of PVA and to yield a negative surface charge (due to the phosphate crosslinking),’ she explains. ‘STMP is a non-toxic crosslinker commonly used to crosslink polysaccharides in the food industry. This PVA and STMP solution was used to 3D print the biomesh.’
In initial trials ‘we observed no visceral adhesion after two and four weeks of the biomesh implantation [in animal models]…We also observed the significantly lower expression of pro-inflammatory cytokines in the biomesh-implanted tissues. This demonstrated that the inflammation-modulating biomesh prevented visceral adhesion formation.’ The next step is to evaluate long-term efficacy.